Causes
(1) Injury caused by puncture
Causes include: ① The puncture incision in the abdominal wall is too small, and excessive force is used to overcome skin resistance during puncture; ② Damaging enlarged or sagging organs by puncturing in the "correct" manner; ③ Patients with a history of abdominal surgery, primary or secondary peritonitis, history of tuberculous peritonitis, or a history of abdominal trauma may have extensive adhesions inside the abdomen. Poor mobility of adhered hollow organs makes them susceptible to injury; ④ Severe gastrointestinal distension. When administering oxygen with a mask or if the endotracheal tube is misplaced into the esophagus, the extremely distended stomach can reach the navel, causing injury.
(2) Conical puncture despite genuine insufflation difficulties
Using the Veress needle closure method to establish pneumoperitoneum, it is unable to detect existing genuine insufflation difficulties. Continuing with the first puncture for conical insufflation ultimately leads to injury to intra-abdominal organs.
(3) Improper use of surgical instruments
Such as excessive traction with forceps causing tearing of the liver, gastric or duodenal walls, or mesentery; inadvertent electrification of the electrocautery tool during surgery, confusion between electrified and non-electrified surgical instruments, or poor coordination during operation causing the electrocautery tool to inadvertently contact nearby organs, resulting in thermal injury to the intestines. Wherry found that 65.52% of intestinal injuries occurred during the initial insertion of instruments into the abdomen, primarily due to injuries from insufflation needles and conical punctures; 27.58% occurred during the dissection process; 6.89% were caused by electrocoagulation and electro section.
(4) Inherent risks of surgical instruments
When separating tissues with laser beams, secondary injuries are easily caused and are now discontinued. Monopolar high-frequency electric knives can also cause intra-abdominal organ damage due to insulation failure, capacitive coupling, direct coupling, and the "skin-seeking effect" within closed body cavities. The recently introduced laparoscopic-specific ultrasonic knife is a safe and efficient cutting tool, with no aerosolization, making it very convenient to use.
(5) Failure to grasp indications and timing for conversion to open surgery
Compared to open surgery, certain inherent limitations of laparoscopic surgery often become very apparent with increasing surgical complexity and lack of experience. At this point, decisively and timely converting to open surgery is often the most crucial means of ensuring surgical safety and quality. Surgeons who have experienced serious surgical complications often have this realization: whether to convert to open surgery in certain situations has become a watershed in determining the success or failure of the surgery.

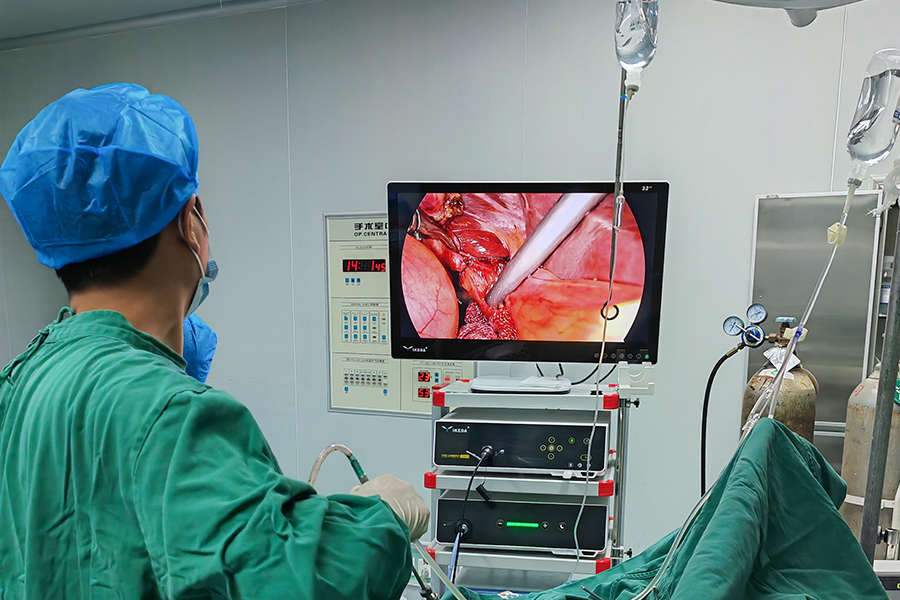
Characteristics and Management
Injuries to internal organs during laparoscopic procedures, depending on the specific organ involved and the time of diagnosis, require diverse treatment approaches.
(1) Injuries to Solid Organs
If injured by the insufflation needle, due to the small extent of the damage, there is often no severe bleeding or signs of hemorrhagic shock, and special treatment is generally not required. If injured by the conical puncture and not discovered promptly during the procedure, patients may experience hemorrhagic shock postoperatively. After diagnosis, abdominal exploration for hemostasis should be performed simultaneously with anti-shock measures. Diaphragmatic muscle injuries often occur in children or due to improper use of electric hooks. Patients may experience shortness of breath and difficulty breathing postoperatively, with chest X-rays showing signs of pneumothorax. If the pneumothorax is minimal, it can be treated with needle aspiration; if the results are unsatisfactory, closed chest drainage may be necessary. Diaphragmatic injuries discovered during the procedure, with small perforations, can conclude the surgery with close postoperative observation. Larger perforations require laparoscopic or open abdominal repair.
(2) Injuries to Hollow Organs
For injuries identified during the procedure, proficient surgeons can perform laparoscopic repairs; otherwise, an open approach may be necessary for the corresponding repair. Perforations of hollow organs not detected during laparoscopic procedures may present clinically in two types postoperatively:
① Overlooking existing perforations of hollow organs during the procedure, early postoperative symptoms and signs of typical peritonitis may occur. However, clinical instances of delayed diagnosis are still common. The most common reason for misdiagnosis is attributing the patient's postoperative complaints to "poor tolerance."
② Electric or laser-induced necrosis, detachment, and delayed perforation of hollow organ tissues. The natural course of such injuries involves a brief period of stable recovery (3 to 5 days) after the operation, during which patients can often resume activities and eating. Subsequently, there is a sudden appearance of typical secondary peritonitis manifestations. Diagnosis based on clinical presentations is not difficult.
Postoperatively diagnosed injuries to hollow organs require specific repairs based on the characteristics of the damaged organ. Injuries to the stomach or jejunum may be repaired in a single stage, while colon injuries may require a one-stage repair or ostomy depending on the time from injury to diagnosis, the severity of abdominal infection, and the overall condition of the patient. Thoroughly irrigating the abdominal cavity, appropriate abdominal drainage, combined antibiotic use, correction of shock, correction of electrolyte imbalances, and correction of acid-base imbalances are all necessary. It is noteworthy to mention duodenal injuries during laparoscopic procedures.
Duodenal injuries during laparoscopic procedures are characterized by subtle symptoms and a high mortality rate. If bile leakage persists after flushing the surgical field, one should not easily conclude gallbladder rupture. Postoperative patients who experience abdominal pain, chills, high fever, and discharge of bile-like substances of varying colors from abdominal drains, possibly accompanied by intestinal fluid or pus, exhibit typical signs of duodenal injury.
Skin corrosion around the abdominal drain, amylase measurement in drain fluid, and observing the color of abdominal drain fluid after oral administration of methylene blue have diagnostic value. Duodenal injuries discovered intraoperatively or in the early postoperative period during laparoscopic procedures should be immediately repaired either laparoscopically or through an open approach. These injuries usually have small wounds and can be cured by one-stage repair. Delayed duodenal fistulas after laparoscopic procedures, with the presence of abdominal drainage, may not exhibit obvious diffuse peritonitis and systemic symptoms. With comprehensive treatment measures such as infection control and parenteral nutrition support while maintaining unobstructed abdominal drainage conditions, cure is possible.
Prevention
(1) Preoperative Preparation
Prior to surgery, palpation and percussion of the liver and spleen area can determine the height of the lower border. For patients with a lower position of the liver and spleen, the first puncture position should be correspondingly lowered. Preoperatively empty the bladder, place a gastric tube for intraoperative gastric and duodenal content suction, reducing the chance of damaging the stomach, duodenum, and bladder. There have been reports of laparoscopic cholecystectomy (LC) cases where a gastric tube was placed preoperatively but gastric contents were not aspirated. After the first puncture, the tip of the gastric tube was found to have entered the abdomen through the gastric perforation. Avoid consuming gas-producing foods such as milk and beans preoperatively to reduce intestinal bloating. Administer an enema in the morning to evacuate feces and gas from the colon, aiding in exposing the surgical field and reducing the chance of colon injury.
(2) Judgment of Intra-abdominal Adhesions Preoperatively and Intraoperatively
Patients with a history of long-term recurrent abdominal pain, primary or secondary peritonitis, tuberculous peritonitis, and upper abdominal surgery, especially those with schistosome liver fibrosis or a history of percutaneous gallbladder stone removal, often have varying degrees of dense adhesions in the abdomen. Preoperatively, ultrasound can indirectly assess whether there are adhesions between the anterior abdominal wall and the viscera, and in some cases, the nature of the adhesions can be determined.
When establishing pneumoperitoneum, patients with a history of upper abdominal surgery should be at least 5.0 cm away from the original incision for the first puncture. If the abdominal muscles are relaxed and the technique is appropriate, but insufflation remains difficult, it indicates extensive adhesions in the abdomen, classified as true insufflation difficulty, and laparoscopic surgery should be terminated. Sometimes, despite intra-abdominal adhesions, insufflation can proceed smoothly after adjusting the position of the insufflation needle, indicating that the adhesions are not severe. However, the surgeon must grasp the direction and depth of the insufflation needle.
(3) Avoiding Violent Puncture
The skin incision for each puncture hole should be slightly larger than the outer diameter of the puncture cone. During puncture, lift both sides of the abdominal wall, rotate the wrist of the right hand, and gently advance the cone without using force. When the puncture sheath enters the abdomen, there is often a feeling of breakthrough twice. After obtaining the second breakthrough sensation, retract the core of the puncture cone first and then push the puncture sheath into the abdomen 3 cm to 5 cm. Sometimes, even when the sheath has reached a considerable depth, there is no clear sensation of two breakthroughs. In such cases, an insufflation tube can be connected to try insufflation to determine if the puncture is correct. Do not blindly puncture deep into the abdomen just to find the two breakthrough sensations. The term "safe cone sheath" does not necessarily guarantee safety. If a "lodged" sensation is felt during puncture, special attention should be paid to potential secondary injuries.
(4) Mastering the Basic Skills of Laparoscopic Surgery
Operating under direct vision in a clear surgical field, coordinated eye-hand-foot coordination, and adept manipulation of surgical instruments are fundamental prerequisites for preventing organ damage. During LC, special attention should be paid to whether there is damage to the upper wall of the duodenum and transverse colon.
(5) Grasping the Indications and Timing for Conversion Surgery
When severe adhesions are discovered, anatomical relationships are unclear, or there is intraoperative uncontrollable intra-abdominal bleeding, conversion surgery should be performed promptly.
(6) Understanding Instrument Performance and Mastering Correct Usage
The "skin-seeking effect" of high-frequency electric current can cause tissue damage in remote areas. Therefore, when cutting adhesions and other tissues, maintain some tension between the tissue being cut and the protected tissue and cut close to the tissue being cut during electrocautery. Laser knives are expensive, operationally complex, and prone to secondary injuries, so they are not suitable for use. In units with the necessary conditions, bipolar electric knives, argon knives, or ultrasonic knives can be used.
(7) Thoroughly Inspecting the Abdominal Cavity Before Completion
At the end of laparoscopic surgery, special attention should be paid to checking whether there is suspicious bile, intestinal fluid, or fecal leakage in the corresponding operative area. For small, gray-white patches of gastrointestinal wall tissue that are not perforated, myometrial layer sutures should be performed to prevent delayed perforation of hollow organs. For suspected injuries to hollow organs, methylene blue can be injected through a nasogastric tube for observation, and a abdominal drainage tube should be placed before the end of the operation for postoperative observation.
(8) Considerations at the End of Surgery
At the end of the operation, retract the instruments from the operating ports under direct vision, then remove the laparoscope last. Open the vent hole of the laparoscope sheath to release accumulated gas in the abdominal cavity, but avoid forcefully compressing the abdominal wall, as this will increase the chance of incisional hernia formation. After removing the final laparoscope sheath, lift both sides of the abdominal wall and perform a shaking motion to facilitate the possible descent of visceral organs (such as intestines) that may have entered the incision, reducing the chance of incisional hernia formation.